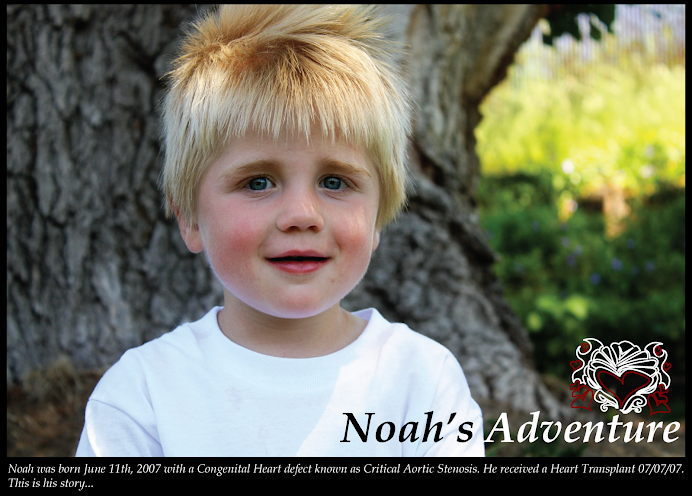
It's been a very long time since I've updated Noah's blog. I guess it's safe to assume all has been going well and I didn't have much to share.
Until this past month that is. The past few weeks have been such an overwhelming experience that I've had to wait until I could process it all before I could share it here. But now that I'm ready to share, I need to start at the beginning to fully chronicle and explain the situation.
In 2010 Noah has his yearly cath in Denver. He hadn't had one in 2 years but had been doing really well. He was only on one immune-suppression med (Neoral) and didn't have any signs of rejection. Unfortunately, his biopsies came back with a cellular rejection level of 1R on the International scale. It was decided that, because he wasn't symptomatic and 1R is very low, we wouldn't do any treatment. But instead of waiting 2 years, he would come back the next year.
Fast forward to 2011. Noah was now on his one immune-suppression med and we had added a blood pressure med to try and help his blood pressure. The morning of his cath (in Denver) we did an Echo and for the first time I noticed his heart rate was all over the place. Ranging between the 40's and the upper 90's. I always watch real close and had never seen this before. Instantly, I was on alert. The only time Noah has ever had rejection before it was right after transplant. His biopsy came back zero but he was having erratic heart rates and arrhythmia's. That eventually lead to PVCs and SVT. Once we treated for rejection, that all cleared up and his heart rate/rhythms went back to normal. So seeing his heart rate jump around was an instant red flag.
My concerns were confirmed when Noah's heart rate dropped dangerously low during the cath procedure requiring meds to bring it back up. The biopsy results came back at a 1R again. This time, we decided we needed to do something. But since Shane and I didn't want to stay in Denver for 3 months for treatment and his level was still really low, we were able to do a 10 day oral steroid taper and see if that would help. We also added a second immune-suppression med (Cellcept). When we came home and followed up with our local hospital Noah's Echo's looked good, his ECG's were okay, but we noticed his heart rate was now sitting in the 60s. Not the 80/90's it previously did during rest.
We continued to watch him closely but in November (3 months after his cath) he developed UTI symptoms that progressed quickly and ended up with Noah peeing blood every 5 minutes and being in a lot pain. Alison (Noah's Transplant Coordinator Super Star) suggested we test for the BK virus. It came back positive. It's a very common virus that the majority of the population are carriers for but without symptoms. In the transplant/immune-suppressed population, it can cause serious symptoms that can lead to Kidney Failure and eventually a kidney transplant.
We had to lower all of his immune-suppression meds and do a round of IVIG (anti-bodies from the blood of 1000 donors) to try and help his body fight off the infection. It became a balancing act of keeping his medication levels low enough that his body could fight this infection and save his kidneys but also high enough that his heart would be protected. (At this time we also found out that Noah has a stage 4 kidney reflux which we will need follow up care.)
We thought we had things under control and Shane and I attributed Noah's increasingly horrible behaviour on all the sensory issues he had dealt with during these tests and treatments. His behaviour continued to get worse but I didn't see any rejection symptoms that had me overly concerned other than his low heart rates. Then toward the end of January Noah stopped eating. I watched closely but thought maybe it was just a phase that would pass. The big sign was that he stopped drinking his carnation bottles too. There have been times when he hasn't eaten very good in the past but he ALWAYS drank his milk with carnations. About two weeks into the no eating, I forced him to eat some breakfast. 5 minutes later he threw up. That is a HUGE warning sign. But we didn't want to rush it in case it was just a tummy bug. The next day, the same thing happened. He had a few bites of breakfast and 5 minutes later he threw up. Now my Warning Sirens were going and I called our Local Transplant Coordinators in a panic.
This is where things get hairy (and the very long story continues).
I called and called and called and couldn't get a hold of anyone. I knew he needed to be seen that day and I was running out of time to get him in there. No one was returning my voice mails and the hospital operator refused to page the on-call coordinator during regular business hours. I FINALLY got a hold of them and they fit him into the schedule.
His echo was the same, his ECG was the same (but low heart rate) but his symptoms were worrisome. But it was decided to send him home and maybe come back again next week. As we left the hospital, I call Alison to keep her updated and she was not happy. His symptoms really worried her and she asked to call me back after she had talked to Dr. Pietra.
When she called me back, I was not at all ready for her response. "Come Now!" She wanted us on a plane that night.
I instantly started questioning myself. Wondering if I was over-reacting. Going to Denver so unexpectedly, possibly staying for several months, what would I do with my other kids.... it was overwhelming. After talking with Shane and knowing that a HUGE snow storm was hitting Denver the next morning and thinking my flight would be delayed anyways, we decided to wait the weekend and if he wasn't better by Monday, we would go. In the mean time, Alison spoke with the team at PCMC and they decided to take the situation a bit more seriously. They now both agreed that we needed to do a heart cath and biopsies. They were also willing to do it here in Salt Lake so we didn't need to go to Denver.
The next day Noah went in for a Heart Cath. PCMC does their biopsy results a bit differently than Denver. In Denver, they rank the cellular rejection on the International scale and then look at the vascular function (like the Coronaries) and the Donor Specific Antibody blood count. At PCMC, they have two scales. A C Scale (Cellular rejection 1-5) and a V Scale (Vascular or Antibody rejection 1-5). Plus they look at the DSA (Donor Specific Antibodies: Antibodies that your body makes specifically targeting the donor organ). This cath showed that his Cellular rejection had gotten better (it was now a 0) but his AMR (Antibody Mediated Rejection was now a V3. The DSA also showed his body was making Donor Specific Antibodies.
Due to his symptoms (low heart rate, not eating, throwing up, looking pale, being tired) and his biopsy results, Noah was admitted to the hospital Friday morning. The plan was for 2 rounds of IVIG and 6 doses of IV Steroids. I went into the treatment expecting his heart rate to return to normal and for him to get better. But watching his heart rate on the monitor that weekend I realized very quickly that it wasn't getting better. It was actually a lot worse than I expected. It was more than just a slow heart rate. Noah was having lots of PVCs, skipped beats, extra beats, and even something that was entirely new to me. Something called Junctional Escape beats (or something like that). I was told that those are the types of beats that can kill you. Your heart just stops beating. As long as he was having them, he couldn't go home.
It was decided that Noah was having something called Sinus Node Dysfunction. (I'll try to explain that: the heart has a built in pacemaker, the part of your heart that makes your heart beat. The first part is the Sinus Node, then it goes to the AV node, then to the bundle of HIS, and on to the bottom of the ventricle [I might be explaining this wrong, don't base your medical degree on my explanation]. The part that is suppose to fire first, the Sinus Node wasn't always working. Normally, the AV node would pick up and start the heart but even then, sometimes it wasn't firing either. This was all causing the super low heart rates and when the AV node miss-fired he was having the escape beats.) Dr. E at PCMC thought this was now a permanent result of the ongoing rejection. She said it wouldn't ever get better and that Noah now needed a pacemaker. Denver said they wanted to try a more aggressive medication route first (which is standard treatment for all rejection there).
Shane and I thought and prayed about it. And while the heavy duty medications scared us (they aren't without risks of their own) we felt that we would rather treat for rejection before assuming it was permanent. As the ONLY way to know for sure that this wasn't going to get better was to try and treat it first.
Dr. E refused. It was her medical opinion that it wasn't going to get better and she basically gave me an ultimatum. PCMC or Denver. But if we chose Denver, ALL his care had to go. They weren't going to even facilitate check ups anymore. That would mean going to Denver every 3-4 months for Echos and routine Dr appointments.
This would have upset me no matter what, but add in the pregnancy hormones and I was a complete mess. I usually stay very analytical and rational during these discussions so that I can process what the Dr's tell me and save my crying for a more private setting. Not this time. I could not stop crying!
You see.... Noah received this amazing gift of life with this new heart at 26 days old. Having it last him even 20 years is all that's been seen so far. My prayers are that it lasts him MUCH longer than that. I pray for a very long lifetime for him without needing another transplant. But to tell me that at 4 1/2 yrs old his heart is already permanently damaged is heart breaking to me.
Dr. E agreed to discuss it with the other transplant Drs in the state the next morning and see if any of them thought it was a good idea to try the medication first. She came back and still said no. I feel like I plead my case as well as I could. I told her that we couldn't go to Denver. There was no way I could split our family up like we did when Noah was born. We had to stay together. So I didn't want them to tell me to chose between them and Denver. What I wanted, was for her to make me feel more comfortable with the Pacer decision. Could we compromise? Was there another step we could take before doing this permanent procedure that wasn't without it's own risks and future complications. I begged, I cried, I pleaded.... and she still said no.
I can't even begin to tell you how this made me feel. But to try.... I felt like my rights as his mother were taken away. We were no longer given a choice. It was their way or the highway. I felt 100% forced into this and it was overwhelming. Didn't my opinion as his mother count for anything? I mean, they wanted to send him HOME in the first place. It was only my concern and Alison's pressuring that even led them to take this whole thing more seriously and yet, now they knew better than all of us. I was angry. But when it came down to it, we had no choice. We couldn't go to Denver and live in a hotel and split up our family or take Lilly out of school... we were stuck.
The procedure was scheduled for the following day. I was told that once they got in and did the testing they would determine if he needed just a sinus node pacer or if he would need a dual chamber (sinus node and AV node pacer). If he needed the dual chamber, he might have to have his chest cracked open to put it in. I was very firm in telling them that if they decided he needed his chest cracked then they had to stop and I WOULD be moving to Denver. (It was a very serious HELL NO).
Luckily, he didn't need that. They had a very hard time placing the lead through his vessels but were finally able to get it placed without complications. He now has a Pace Maker in his upper left shoulder that paces his heart at 80 beats per minute. While resting, it paces 100% of the time. I'll find out during further testing how much his heart beats on it's own while he's active.
The entire stay was very hard on him but he did surprisingly well. The hardest part was getting the IVs. Right before his pacer procedure they needed to place another IV. I requested the best of the IV team (but I don't think they sent the best). They tried twice and couldn't get it in and I told them they had to stop. They would have to place it after he was asleep in the cath lab. Afterwards he was SO upset. He looked at me and asked if he could have a carnations. But since he was going in for surgery he wasn't allowed and I had to tell him no. It was the saddest thing. He wasn't scared or freaking out. He was utterly and completely sad and pulled the blanket up over his face to cover his emotional pain. Just thinking about it makes me cry. I climbed into bed with him as I bawled and hugged him tight. The poor boy has to go through so much. Sometimes I just seems like too much. I wish I could do it all for him.
After being in the hospital for an entire week, he finally got to come home. He came home on 13 medications including increased immune-suppression levels and an Oral Steroid taper. His next cath and heart biopsies was scheduled for a week and a half later.
That was three days ago. Results came back that showed he was still a V3 and his DSA hadn't changed. Not better but not worse either. It was decided to keep him on the steroids a bit longer, proceed with the IVIG infusions once a month and recath him in 6-8 weeks and check the rejection level again then. If symptoms get worse, his pacer has to pace him 100% (showing his heart isn't beating well at all on it's own) or if the biopsies show increased rejection during the next cath we will need to treat it more aggressively. The plan would most likely be ATG (a super immune-suppression med that lasts nearly a year and suppresses the T cells that can cause antibodies) and a procedure called Plasmapheresis (which is like dialysis for the blood but gets rid of existing antibodies). I hear the Plasmapheresis is horrible and I REALLY hope this rejection clears up on its own.
This whole situation has been overwhelming. Not only is it hard enough to face the reality of Noah rejecting his heart and having it damaged and needing a pacemaker but add on top of that feeling pressured into a treatment we weren't ready for and this past month has been horrid. All the hormones I have going on right now have made it even harder. But I'm trying really hard to come to terms with it all and not be angry at the hospital. I know that they were just doing what they felt was best. I just wish things could have played out a bit differently.
Shane and I both prayed that whatever was best for Noah would happen. And since the choice of treatment was taken away from us, all we can do is have faith that what ended up happening was for the best. Ultimately, we have to put it all in God's hands and trust that He is protecting and watching out for my little man.
One good thing that has come of all this though is that Noah is feeling better with his heart rate not being so low. His behavior has gone back to a manageable level of freak outs. But best of all, he has started giving kisses and hugs again. And even tells me he loves me. It has been MONTHS since he has felt well enough to show any form of kindness.
The day after he got released from the hospital he came up to me and told me how he was going to play with all of his trains at home while Mom and Dad and YeeYee and Bay Aayee were all home too. Then he says "I so hapeee!" Talk about melting my heart! Then a few days ago he was saying Mom? Mom? Mom? I said, Whattrains at home while Mom and Dad and YeeYee and Bay Aayee were all home too. Then he says "I so hapeee!" Talk about melting my heart! Then a few days ago he was saying Mom? Mom? Mom? I said, What Noah? and he replied "I ove ooo!"
I ove ooo too my sweet sweet boy.
![]()
Friday, February 24, 2012
Rejection, A Pacemaker, and Lots of Tears
With Much Love, Crystal at 5:17 PM
Subscribe to:
Post Comments (Atom)







My heart just aches for you guys! I can't believe the way parents are often treated by the medical field. :( I am so sorry your options were so stunted and limited by the doctor! I also pray that it was all for the best- that our Heavenly Father is doing what is best for little Noah! I don't blame you for not wanting to go to Denver! I think you have got to be the worlds strongest Mom...and I applaud you for fighting for your family and for what you and your hubby feel is RIGHT for your family! I love you guys! I pray for you all..if you need ANYTHING, please, never hesitate to ask!!! Love to you little Noah!
ReplyDeleteWow! I am glad the pacer is helping him feel better. Hopefully the rejection will get under control. I wish for your sakes that your experience would have been better, but I love your faith and trust in God's plan for your sweet little man. You are an awesome momma!
ReplyDeleteOkay, now I am bawling after reading your post!! I was blog surfing my heart friends and came across your blog. 1st of all I am so sorry you as parents were put in that position. I feel so sad and angry. Kylie is HLHS with heart failure, I have already made up my mind once she cross's transplant no going back we are going to try and leave PCMC. I don't feel confident in the program there and after reading your post, that just confirmed how I fell. I am so heartbroken over this. I am glad he is doing better though. What you said about his behavior changing, then eating going down, makes me worry for Kylie she has major attitude issue's (which I am thinking she doesn't feel good either) and now her not wanting her beebaahs (bottle) makes me worry!! I am so glad I came across your blog!! Hope you don't mind me following it. I am glad you posted an update!! Lots of prayers headed your way!!!
ReplyDelete